Total Shoulder Replacement Surgery: Benefits, Risks, and What to Expect
Just like the knee and hip, the shoulder joint is susceptible to wear and tear, and may eventually need to be replaced, especially if you suffer from osteoporosis or have experienced a trauma to the bone.
Here are some answers to common questions about the procedure.
When do you potentially need a shoulder replacement?
- When your shoulder consistently gives you pain
- When movement has become too restrictive
- When it no longer responds to such treatments as physical therapy and medications, including pain-relieving injections
What are the causes of these shoulder conditions?
- Osteoarthritis
- Rheumatoid Arthritis
- Posttraumatic Arthritis
- Rotator Cuff Tear Arthropathy
- Avascular Necrosis
- Severe Injury
Who is a likely candidate for the surgery?
- General good health
- Appropriate weight (BMI <40)
- Non-smoker
- Arthritis that has failed to respond to conservative treatment
How common is shoulder surgery?
Shoulder joint replacement has become increasingly common, and is now as effective as knee and hip replacement surgery to help patients get back to their normal activities without pain. According to the Journal of Shoulder and Elbow Surgery, 175,000 to 350,000 procedures per year may be performed by 2025. Orthopedic Performance Institute surgeons, Dr. Matthew Dwyer and Dr. Christopher Phelps, routinely perform shoulder replacement surgery.
How is it done?
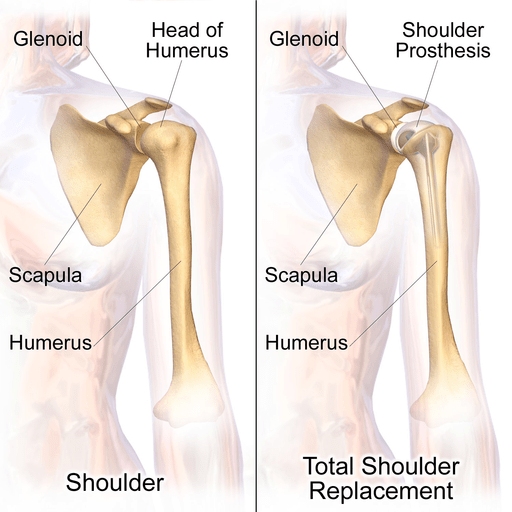
Total shoulder replacement surgery, also known as shoulder arthroplasty, involves removing the damaged portions of the shoulder joint and replacing them with artificial components, collectively referred to as a prosthesis.
The surgeon begins by making an incision over the shoulder to access the joint. The damaged or arthritic cartilage and bone from the head of the humerus (the upper arm bone) and sometimes the socket of the scapula (the glenoid) are carefully removed. These surfaces are then reshaped to fit the prosthetic components.
The artificial joint is made from metal and plastic materials designed to mimic the natural anatomy and function of the shoulder. Cement or a press-fit technique may be used to secure the prosthesis, depending on bone quality and the specific implant design.
Replacement Options
There are different types of shoulder replacement procedures, depending on the extent of joint damage and the patient’s needs:
- Partial Shoulder Replacement (Hemiarthroplasty)
In this procedure, only the head of the humerus (the “ball” of the joint) is replaced with a metal implant. The socket (glenoid) is left intact. This option is often chosen when the glenoid is healthy or when the damage is primarily limited to the humeral head, such as in some fractures. - Total Shoulder Replacement (Anatomic Total Shoulder Arthroplasty)
Both the ball (humeral head) and the socket (glenoid) are replaced. The humeral component is typically metal, while the glenoid component is made of medical-grade plastic (polyethylene). This is the most common type of shoulder replacement and is generally recommended for patients with osteoarthritis, rheumatoid arthritis, or severe joint damage. - Reverse Shoulder Replacement (Reverse Total Shoulder Arthroplasty)
In cases where the rotator cuff is severely damaged or nonfunctional, a reverse shoulder replacement may be used. This procedure reverses the normal ball-and-socket configuration: a metal ball is attached to the scapula, and a plastic socket is placed on the top of the humerus. This design relies on the deltoid muscle rather than the rotator cuff to lift the arm, making it ideal for patients with rotator cuff arthropathy.
Your orthopedic surgeon will determine which course of action to take.
What evaluation processes are involved?
The Orthopedic Performance Institute’s Dr. Matthew Dwyer and Dr. Christopher Phelps will evaluate you in four key areas.
- Medical history. You’ll be asked about your overall health, pain and ability to perform everyday activities.
- Physical examination. This will assess your shoulder motion ad strength.
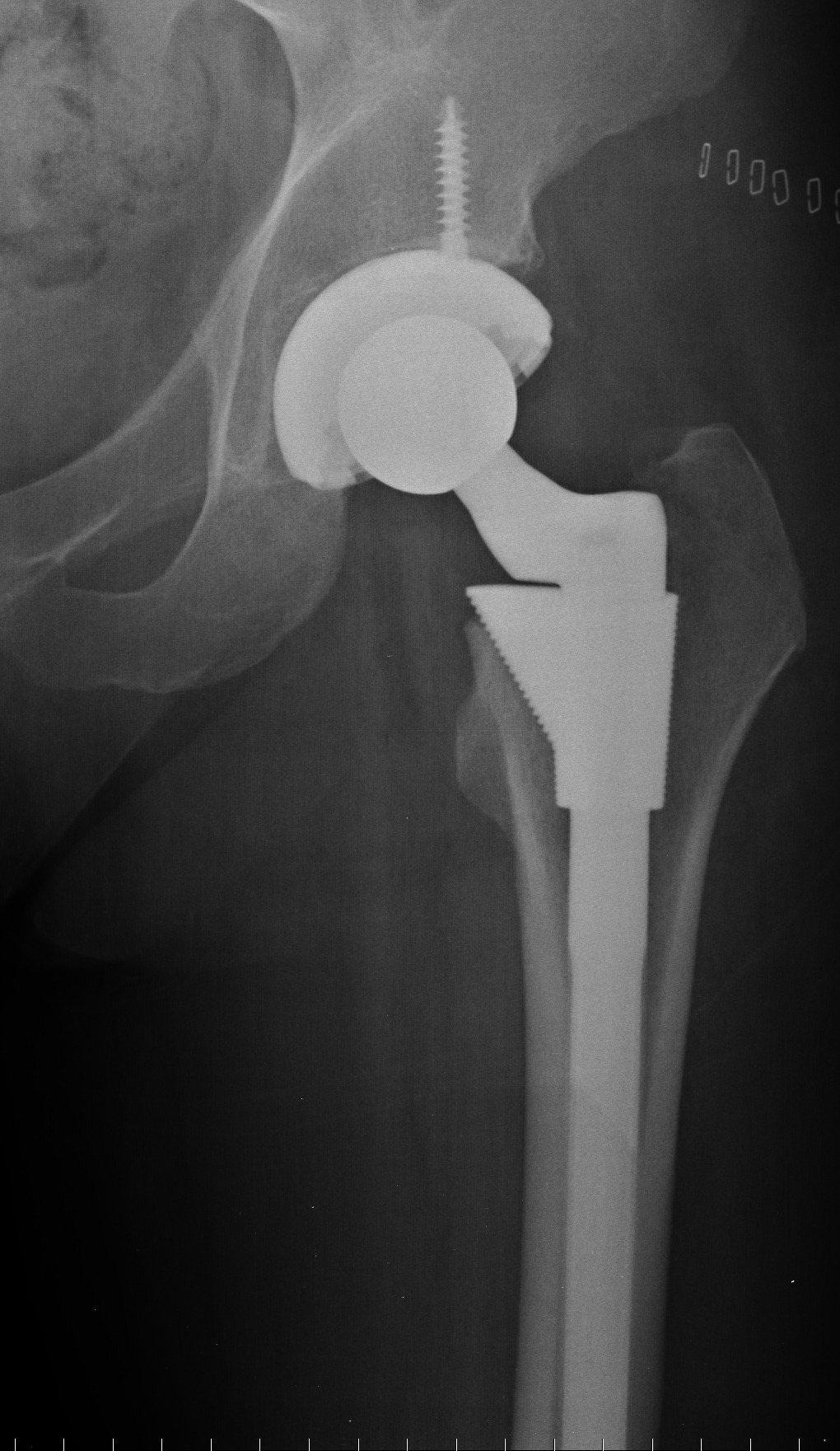
- X-rays. These will allow the doctors to evaluate the damage and what needs to be replaced.
- CT scans and MRIs. These procedures may be warranted to allow a closer examination of the bone and soft tissue.
How long is the surgery?
The procedure is typically performed under general anesthesia and may take about 1.5 to 3 hours, depending on the complexity. Afterwards, you will either be released home or be admitted to the hospital for further observation.
What is the recovery timetable?
Recovery from shoulder surgery is a gradual process that typically spans about a year. In the first 1–2 weeks, patients begin gentle home physical therapy focused on passive range of motion, while keeping the shoulder dry until the surgical dressing is removed during the two-week follow-up. Sling immobilization is crucial during the first six weeks. From weeks 2–6, outpatient physical therapy continues to focus on passive motion, still with sling use. Between weeks 6–10, patients can discontinue the sling and begin active range of motion exercises, avoiding any lifting. From weeks 10–14, therapy progresses to include strengthening exercises. By 3–6 months, most patients follow a home regimen to further improve motion and build strength. Full recovery is typically achieved around one year post-surgery.
Contact Us Today
Don’t let shoulder pain keep you from the activities you love. Contact the Orthopedic Performance Institute in San Antonio at (210) 545-7171 for a complete evaluation with Dr. Christopher Phelps or Dr. Matthew Dwyer.

 Next Post
Next Post