Hip Replacement FAQs
Your chances of osteoarthritis of the weightbearing joints of the knee and hip increase with age; the condition most often affects middle-aged and older people. Osteoarthritis may first appear between the ages of 30 and 40, though symptoms may not be present in the early stages. Later in life, many Americans will experience joint pain due to arthritis that can make enjoying life very challenging.
When do I need a hip replacement?
When traditional, non-surgical treatment options have failed to manage the pain from an arthritic hip, joint replacement (arthroplasty) can be a valuable tool. The surgeons and staff at Orthopedic Performance Institute are dedicated to combating the effects of osteoarthritis and are determined to guide patients back to an active, enjoyable lifestyle.
We combine patient preparation with advanced surgical techniques, innovative pain management tools, and enhanced rehabilitation strategies to revitalize the lives of patients every day. The foundation of our program is extensive patient education coupled with comprehensive support to ensure success from the beginning. Prepare to excel!
What does a hip replacement involve?
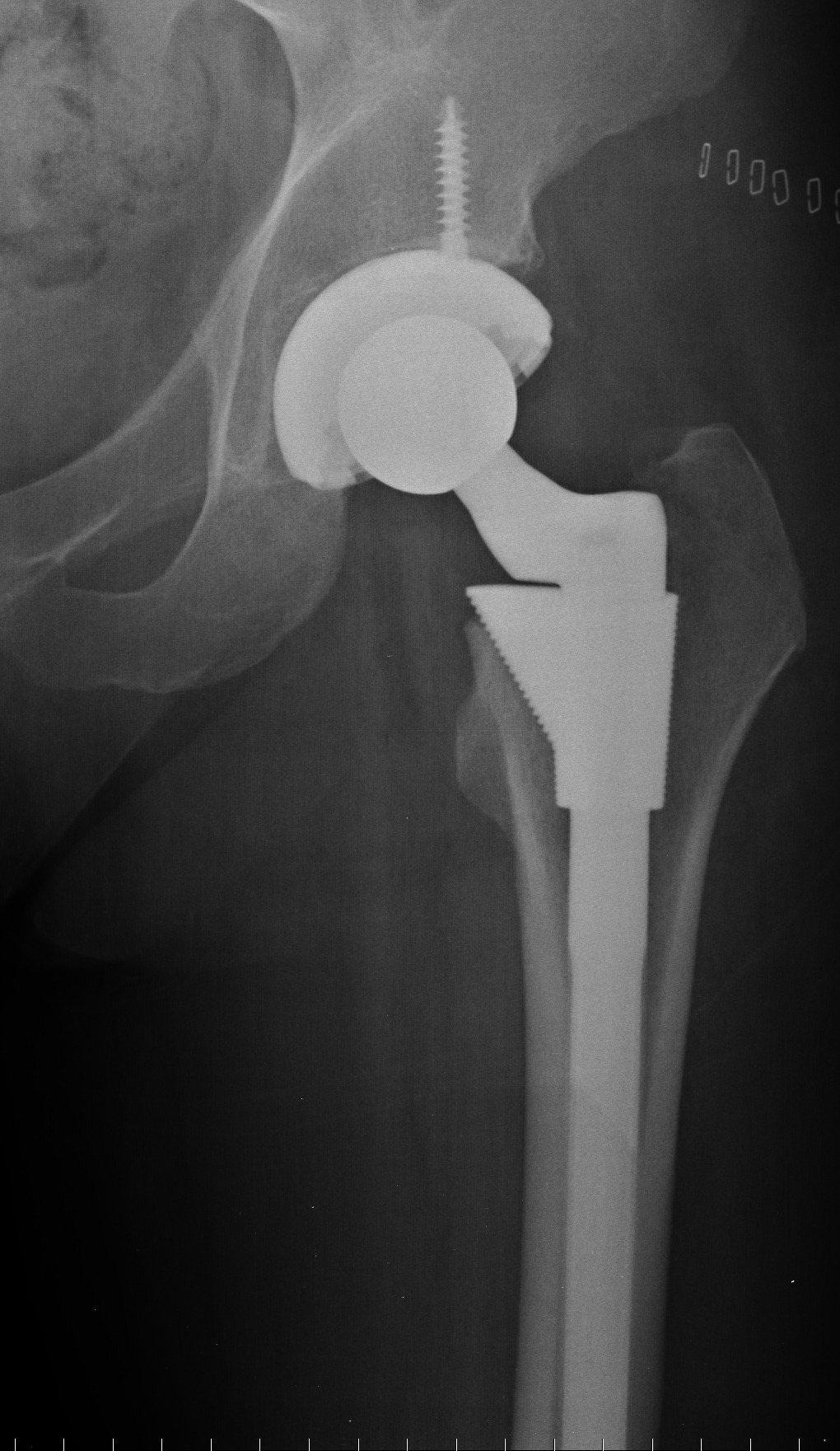
In a total hip replacement (also called total hip arthroplasty), the damaged bone and cartilage is removed and replaced with prosthetic components.
- The damaged femoral head is removed and replaced with a metal stem that is placed into the hollow center of the femur. The femoral stem may be either cemented or “press fit” into the bone.
- A metal or ceramic ball is placed on the upper part of the stem. This ball replaces the
damaged femoral head that was removed. - The damaged cartilage surface of the socket (acetabulum) is removed and replaced with a metal socket. Screws or cement are sometimes used to hold the socket in place.
- A plastic spacer is inserted between the new ball and the socket to allow for a smooth gliding surface.
A successful recovery is accomplished through extensive patient education and preparation combined with minimally invasive surgical techniques, advanced pain management therapies and rehabilitative support. Surgery itself takes about 1.5 hours; patients should plan to be up and walking with the therapist in the hospital on the day of surgery.
How is pain managed during surgery?
General anesthesia, given by IV, is administered by the anesthesiologist for surgery. Oral medications and additional injectable medications may be given as needed for pain or relaxation.
When should I expect to go home?
Patients should plan on a 1-2 night hospital stay after hip replacement surgery. We then allow the patient to fully recover at home with the assistance of in-home physical therapy and nursing
services as needed. Most patients are discharged with oral pain medication. These medications, when taken as directed, typically provide excellent pain relief at home. A physical therapist will walk with you prior to discharge from the hospital to ensure you are stable and comfortable.
Who is a good candidate for outpatient joint replacement surgery?
The success of total joint replacement surgery is dependent on several factors. One of the most imperative factors is preparation and education of the patient. Our team is dedicated to ensuring our patients achieve their goals of returning to an active, pain free lifestyle but your
understanding, participation and commitment are imperative to the success of your procedure. These guidelines are the basis of our patient selection strategy for joint replacement surgery. Speak with one of our experienced providers to determine if you are a good candidate for joint replacement surgery.
| • Good health | • Appropriate body weight (BMI <40) |
| • Non-smoker | • Arthritis that has failed to respond to conservative treatment |
What are the risks associated with joint replacement surgery?
Our surgeons perform hundreds of successful joint replacement surgeries each year and our staff is dedicated to the safety of each of our patients. However, there are potential complications associated with any surgery. Below are some of the risks associated with joint replacement surgery and the precautions we take to minimize these concerns.
Infection. Prior to surgery, your pre-operative testing will help identify active infections and potential sources of infection. These will be treated appropriately. Surgery will not take place if there is any potential active infection present (ex. skin wounds, respiratory infections, bladder infections). During surgery, our team follows meticulous sterile technique. Patients are treated with IV antibiotics and the surgical site is thoroughly cleansed. Post-operatively, we provide detailed instructions regarding wound care and recommend avoiding dental procedures for six months, including routine cleanings due to the increased risk of joint infection.
Blood Clots. Notify our staff prior to your surgery if you have a history of blood clots. After surgery, you will take Aspirin two times daily. We encourage early walking and regular activity. Compression stockings and foot/ankle pumps can also be helpful in decreasing clotting risk and improving lower leg swelling. We offer Sequential Compression Devices (SCD) for purchase ($225). This simple, battery powered device gently squeezes the lower leg to encourage blood flow and decrease the risk of clotting. Our knowledgeable staff will educate and fit you with this device prior to surgery.
Additional risks associated with every surgery do exist and include numbness, pain, blood vessel or nerve injury, and complications associated with general anesthesia. Expect to have a localized area of numbness near the incision that will remain indefinitely. This is a change in sensation due to the nature of the incision and does not lead to pain or a loss of function.
What can I do to prepare for surgery?
Your health. Our team is always available to provide patients with step by step guidance through the process of joint replacement surgery and recovery, but a successful outcome is dependent on patient preparation and participation.
- Assemble a packet of your medical and personal information, including copies of insurance, health directives, etc. This information can be brought with you to the hospital as well.
- Avoid alcohol use at least 48 hours before surgery.
- Avoid/quit tobacco use as soon as possible.
- If you are in need of any dental work, such as an extraction or periodontal treatment, schedule it well in advance of your surgery. Due to the risk of infection, no dental work is allowed, including routine cleanings, for six months after surgery.
If you’d like to be evaluated as a candidate for hip replacement surgery, contact the Orthopedic Performance Institute.

 Previous Post
Previous Post Next Post
Next Post




