
 What is osteoarthritis?
What is osteoarthritis?Arthritis is a general term that means inflammation of the joints. There are dozens of types of arthritis. Osteoarthritis is the most common type.
OA can be caused by a range of factors that include excess weight, joint injury, and aging (usually after 40). Any joint can be affected by OA, but it occurs most frequently in the hands, knees, hips, and spine.
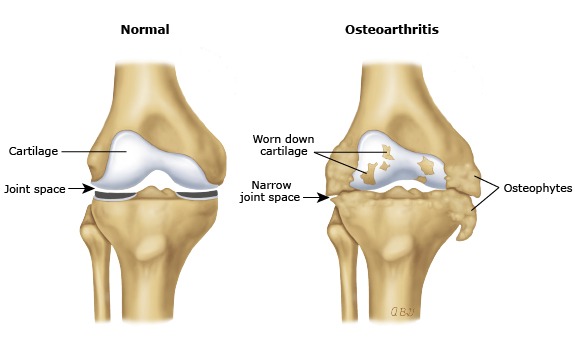
The place where 2 bones meet is normally covered with a rubbery material called cartilage. This material allows the bones to slide over each without causing pain. When osteoarthritis sets in, the cartilage begins to break down. As it wears away, the bones in the joint start to rub against each other. This can cause pain, stiffness, and swelling.
OA is a chronic condition that gradually worsens over time; however, there are several measures that may slow its progression and control symptoms. Diagnosis of OA by a sports medicine specialist or orthopedist is the first step in ensuring the appropriate treatment of OA.

The knee is a target site for OA and worldwide is the commonest single cause of lower-limb disability. It is a degenerative, “wear-and-tear” type of arthritis that occurs most often in people 50 years of age and older, but may occur in younger people, too. While age is a major risk factor for osteoarthritis of the knee, young people can get it, too. For some individuals, it may be hereditary. For others, osteoarthritis of the knee can result from injury or infection or even from being overweight

Patients who have osteoarthritis of the hip sometimes have problems walking, pain, aching, stiffness, and restricted movement. Diagnosis by a sports medicine specialist or orthopedist is necessary because it can be hard to diagnose as pain can appear in different locations, including the groin, thigh, buttocks, or knee. The pain can be stabbing and sharp or it can be a dull ache, and the hip is often stiff.

Osteoarthritis of the shoulder most often occurs in people who are over age 50. In younger people, osteoarthritis can result from an injury or trauma, such as a fractured or dislocated shoulder. This is known as posttraumatic arthritis. Osteoarthritis may also be hereditary.
The shoulder is made up of two joints, the acromioclavicular (AC) joint and the glenohumeral joint. The AC joint is the point osteoarthritis is more commonly found in, where the collarbone, or clavicle, meets the acromion, which is the tip of the shoulder blade.

Our OA treatment is tailored to you and based upon how severe your pain and stiffness are, which joints are affected, how much difficulty you are having with daily activities, and your preferences.
What is it?
The complete arthritis treatment plan is an individualized six-week program to maximize relief and decrease pain from osteoarthritis.
Who can benefit from this program?
Anyone suffering from joint pain due to arthritis, especially those looking for a structured, routine program will benefit. This program is also specific for those who are looking for non-operative management of their OA, or are not able at this time to have a joint replacement.
Will my insurance cover the treatment plan?
This program is designed to be covered by almost all insurances, has lots of research to support the use, and is the primary go-to treatment for OA. Insurance coverage verification is recommended prior to beginning treatment.
What Is Platelet-rich Plasma (PRP)?
Although blood is mainly a liquid (called plasma), it also contains small solid components (red cells, white cells, and platelets.) The platelets are best known for their importance in clotting blood. However, platelets also contain hundreds of proteins called growth factors which are very important in the healing of injuries.
PRP is plasma with many more platelets than what is typically found in blood. The concentration of platelets — and, thereby, the concentration of growth factors — can be 5 to 10 times greater (or richer) than usual.
To develop a PRP preparation, blood must first be drawn from a patient. The platelets are separated from other blood cells and their concentration is increased during a process called centrifugation. Then the increased concentration of platelets is combined with the remaining blood.
How Does PRP Work?
Although it is not exactly clear how PRP works, laboratory studies have shown that the increased concentration of growth factors in PRP can potentially speed up the healing process.
To speed healing, the injury site is treated with the PRP preparation. This can be done in one of two ways:
What Conditions are Treated with PRP and Is It Effective?
Research studies are currently being conducted to evaluate the effectiveness of PRP treatment. At this time, the results of these studies are inconclusive because the effectiveness of PRP therapy can vary. Factors that can influence the effectiveness of PRP treatment include:
STONE OAK
Dr. Matthew Dwyer
Dr. Christopher Phelps
1139 E Sonterra Blvd.,
Suite 500
San Antonio, TX 78258
P: (210) 545-7171
F: (210) 545-7176
In the V. Benson Pavilion connected to Methodist Stone Oak Hospital
SPORTS MEDICINE CLINIC
Dr. Alexandra Matthews
255 East Sonterra Blvd.,
Suite 110
San Antonio, TX 78258
P: (210) 545-7171
F: (210) 545-7176
BOERNE
Dr. Matthew Dwyer
134 Menger Springs,
Suite 1210
Boerne, TX 78006
P: (210) 545-7171
F: (210) 545-7176
PHYSICAL THERAPY CLINIC
255 East Sonterra Blvd.,
Suite 110
San Antonio, TX 78258
P: (210) 545-7171, ext. 301
F: (210) 545-7176
Copyright © 2024 Orthopedic Performance - San Antonio's Board Certified Orthopedic Specialists | Privacy Policy
San Antonio Website Design by Strottner Designs, LLC